A Critical Analysis of the Biopsychosocial Risks Associated with Postpartum Depression in Indian Mothers
By
2021, Vol. 13 No. 02 | pg. 1/1
IN THIS ARTICLE
KEYWORDS
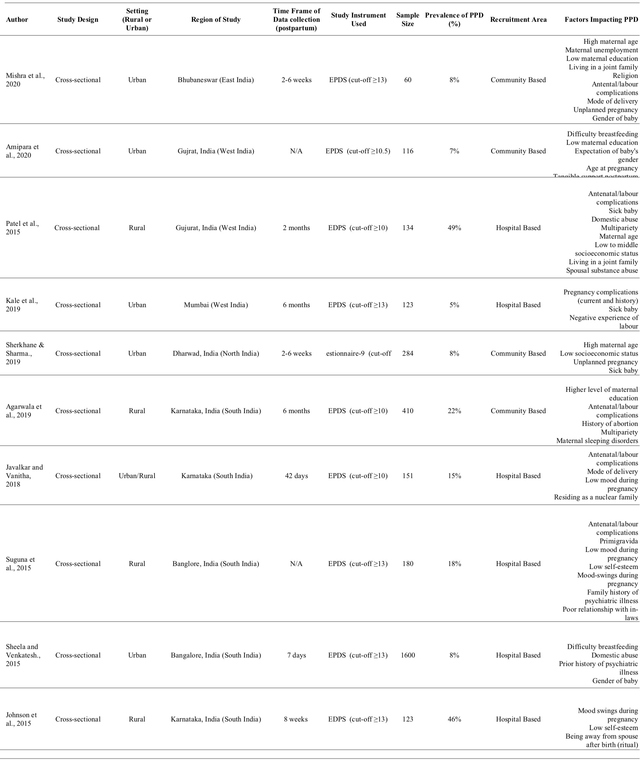
AbstractMotherhood is an essential yet challenging feat that requires constant emotional, social, and physical support. Postpartum depression (PPD) is a devastating illness that has detrimental effects on both the mother and her child. PPD is a growing problem in developing countries such as India, where populations are unaware and unaccepting of mental illnesses. Existing literature has identified several biological and psychological factors contributing to PPD. Interventions and public health policies have been motivated by recognized factors; however, they have not been as successful at reducing rates of PPD. This paper aims to investigate and critically analyze the causes and risks associated with the high prevalence rate of PPD in India. Searches were conducted using relevant MeSH terms on the Queen's University OVID Health and Life Sciences Database Service. The platform was used to search databases including MEDLINE, EMBASE, Global Health, APA PsycInfo, and Joanna Briggs Institute. Additionally, CINAHL and PubMed were searched. Ten studies that matched the inclusion and exclusion criteria were thoroughly analyzed for various factors contributing to PPD. The risk factors were characterized into four categories: biological and obstetric, psychological, familial and cultural, and socio-demographic factors. The reported prevalence rates of PPD amongst the ten studies had an extensive range of 7% - 48%. Additionally, the studies disagreed with each other on which factors significantly increased the risk of PPD in Indian mothers. There are limited sources exploring the cultural and religious factors associated with PPD. Future research must focus on the relationship between cultural and biopsychosocial elements as this may lead to the formation of successful and culturally sensitive interventions. IntroductionPostpartum depression (PPD) is becoming globally prevalent, with about one in seven women diagnosed with the disorder within the first year after childbirth (Wisner, Sit et al., 2013). PPD is described as depressive episodes and mood swings occurring as soon as four weeks post-birth or as a continuation of antenatal depression (Stewart et al., 2003; Wisner, Moses-Kolko et al., 2010). This disorder leads to devastating outcomes such as decreased affectionate interactions between mother and child, which may predispose the mother to chronic depression and negatively influence the growth and development of the infant (Field, 2010; Wisner, Sit et al., 2013). Postpartum depression has been shown to have an uneven world prevalence since the burden of PPD is higher in lower-middle-income countries like India (Fisher et al., 2011). Thus, this paper aims to critically analyze the biological, social, psychological, and social risks associated with PPD while suggesting improvements for future intervention in India. The focus on maternal mental health has not become an integral part of India's health care, despite India's national mental health program enacted in 1982 (Upadhyay et al., 2017). National statistics on PPD in Indian mothers is lacking as data is limited to specific geographic regions (Upadhyay et al., 2017). The overall aggregated prevalence of PPD in Indian mothers is estimated to be 22%, with the highest prevalence in urban areas (24%) and the southern regions (26%) such as Tamil Nadu, Mysore, Karnataka, Goa, Bangalore (Upadhyay et al., 2017). Southern areas may have a higher prevalence due to increased urban slums and domestic violence levels (Upadhyay et al., 2017). The higher prevalence of PPD in urban areas may be due to over-crowding, higher living costs, and tremendous pressure on working mothers. Overall high PPD rates in India may result from specific geographical factors, including low education, low socioeconomic status (SES), or high poverty rates.Although Indian and Western women experience shared risk factors for PPD such as poor marital relationships, antenatal depression, lack of spousal support, or domestic violence; cultural factors such as the gender of the child may explain the relatively high rates of PPD in India (Chandra, 2004; Rahman et al., 2003; Wisner, Sit et al., 2013). A girl's birth is not preferred in India as she is typically considered a burden to her parents (Chandra, 2004). This is due to the financial liability of her dowry and because she cannot be considered the successor of her family lineage (Chandra, 2004; Rahman et al., 2003). Thus, there are expectations for a woman to deliver a male child (Gupta et al., 2013; Rao et al., 2015). Discrimination against a female child may lead to feticide or infanticide, a common practice along the 'infanticide belt' including Tamil Nadu, where there is a higher prevalence of PPD (Rao et al., 2015; Upadhyay et al., 2017). Additionally, India's cultural constructs have set expectations for "good" mothers, which leads to stigma when they are not followed. Childbirth is labeled as the happiest time in a woman's life; thus, feelings of anxiety or sorrow are considered taboo (Upadhyay et al., 2017). Deviations from these norms, along with the frustrations of motherhood, may lead to feelings of guilt. Therefore, help-seeking behaviors are low in India's southern and urban regions as breaking this taboo can lead to a loss of reputation within the community (Upadhyay et al., 2017). Breaking this taboo may further result in social exclusion, discontinuation of financial resources essential for livelihood, or even marital separation (Thippeswamy et al., 2018; Upadhyay et al., 2017; Williams et al., 2017). These factors demonstrate how culture fuels stigma against mental health, resulting in alienation from society. Furthermore, low accessibility to resources and training may reduce the recognition and management of PPD among healthcare professionals. In comparison to Western nations, mothers in India can be discharged within 48 hours after delivery, with even shorter admission durations in publicly funded hospitals (Kumar & Dhillon, 2020). Short hospital stays may not provide sufficient time to recognize signs of PPD and consult with the mother about her feelings. Furthermore, home-observance or post-natal support is focused on infant health rather than the mothers' (Upadhyay et al., 2017). Thus, it is vital to find culturally appropriate interventions that will increase awareness and normalcy of PPD, allowing for improved diagnosis and management. This review will address the risks and causes associated with PPD in Indian mothers. The existing literature will be analyzed to investigate the various risk factors associated with PPD, including biopsychosocial and cultural factors. The aim is to gather data on the causes of the high prevalence rates of postpartum depression in Indian mothers from various regions, thereby identifying potential gaps in the literature that may be filled with recommendations of future interventions that are culturally sensitive. It is crucial to increase awareness of PPD amongst Indian communities and physicians, so women in India may be treated for PPD and other maternal mental illnesses without shame. MethodsThe Queen’s University OVID platform, consisting of MEDLINE, Embase, Global Health, APA PsycInfo, Joanna Briggs Institute, CINAHL, and PubMed were searched for articles related to postpartum depression in India. Search terms included keywords and MeSH terms such as ‘postpartum depression’, ‘India’, ‘maternal outcomes’, ‘infant-maternal relationship’, ‘cultural influence’, ‘stigma’, and ‘mental health’. Study Selection and ExtractionThe inclusion and exclusion criteria were outlined before beginning the preliminary search. The inclusion criteria consisted of cross-sectional and cohort studies published between 2015 and 2020. Studies were included if they (a) analyzed the risk of PPD in women in India, (b) mentioned the specific region the study was conducted in (urban or rural), and (c) provided full-text access. Studies analyzing mothers with chronic illnesses were not included. Any studies that were not in English were not included. After the studies' initial abstract and title screening, a full-text review was conducted to find eligible papers. Table 1: Risk factors associated with postpartum depression in India. ResultsThe search strategy resulted in 171 studies. Subsequently, 159 were excluded because they did not fit the inclusion criteria. The remaining studies were individually analyzed after ensuring they matched the inclusion criteria. The ten studies analyzed various regions of India: North India (10.0%; n=1), East India (10.0%; n=1), West India (30.0%; n=3), and South India (50.0; n=5). The studies looked at both urban (50.0%; n=5), rural (40.0%; n=4), and mixed (10.0%; n=1) populations. The sample sizes in the studies ranged from 60 to 1600 (Table 1). The sample population was collected from either hospitals/antenatal care clinics (60.0%; n=6) or from community-based centers (40.0%; n=4). The time frame of data collection ranged from 7 days to a year postpartum, with two studies not stating the data collection time. Measurement Tools Used in StudiesThe primary measurement tool used to assess PPD is the Edinburgh Postnatal Depression Scale (EPDS) (90.0%; n=9). The EPDS is a self-reported questionnaire that assesses ten items focusing on the mother’s feelings over the past week. It has been used to assesses depressive symptoms pre-and postnatally. The EPDS has shown to be successful in assessing depressive symptoms as it has a sensitivity of 86%, a specificity of 78%, and overall reliability of 0.79 (Cox e al., 1987). The EPDS was translated to the specific language of each region, including Kannada and Hindi. A total score above thirteen indicates a depressive illness; however, not all of the studies included in this paper followed this cut-off (Cox et al.,1987). The Patient Health Questionnaire PHQ-9 was also used (10.0%; n=1), a self-reported diagnostic tool employing the DSM-IV criteria. The questionnaire consists of 9 items, which score from zero to three, with higher numbers indicating increasing symptom occurrence. PHQ-9 has a sensitivity and specificity of 88% for assessing depression severity (Kroenke et al., 2001). Risk FactorsThe risk factors associated with PPD in Indian mothers can be characterized into four categories: biological and obstetric, psychological, familial and cultural, and socio-demographic factors. Biological and Obstetric FactorsTen studies discussed biological and obstetric factors that increase the risk of PPD in India. Increased risk of PPD and presentation of depressive symptoms were associated with high-risk pregnancies (Agarwala et al., 2019; Javalkar &Vanitha, 2018; Kale et al., 2019; Mishra et al., 2020; Suguna et al., 2015). Conditions that cause pregnancies to be labeled high risk include the onset of oligohydramnios, preeclampsia, intrauterine fetal demise, hypertension, gestational diabetes, a history of obstetric complication, rheumatic heart disease, and Rh incompatibility (Javalkar &Vanitha, 2018; Kale et al., 2019; Suguna et al., 2015). A study conducted by Agarwala et al. (2019) found that labor complications increased the risk of PPD development by 10.7 times compared to mothers with healthy parturition. Increased risk of PPD during complicated pregnancies may result from higher levels of stress and anxiety antenatally and postnatally. Out of the studies that analyzed obstetric factors, one did not see a significant correlation between the risk of PPD and antenatal complications (Sheela & Venkatesh, 2015). This inconsistency may be due to small sample sizes and the regional difference in the quality of life, accessibility to healthy food, and the number of daily stressors. Antenatal complications may influence the mode of delivery. Existing or prior history of cesarean-sections (C-section) was found to be associated with PPD symptoms (Javalkar &Vanitha, 2018; Mishra et al., 2020; Sherkhane & Sharma., 2019; Suguna et al., 2015). C-sections may increase stress levels as the mother may be unable to tend to the new baby, other children, or other responsibilities. Moreover, it has been found that discrepancies between the mother’s expectation and the actual pregnancy events, including the mode and time of birth, may impact the occurrence of PPD (Ghaedrahmati et al., 2017). However, one of the studies analyzed did not find a significant association between delivery mode and PPD (Sheela & Venkatesh, 2015). Additionally, studies found that mothers who have premature babies with low birth weight are more likely to be diagnosed with PPD (Patel et al., 2015; Sherkhane & Sharma., 2019). Premature babies may require prolonged hospitalization as they are typically at risk for congenital health problems, which can be costly and may increase maternal stress levels (Kale et al., 2019; Sherkhane & Sharma., 2019). The lack of agreement amongst studies about the mode of the delivery being a significant risk factor may have occurred due to differences in SES, regional costs for hospitalizations and delivery procedures, and the sample size between the studies. Difficulty breastfeeding may be associated with higher risks of PPD because of potential guilt due to feelings of failures of motherhood’s internal and societal expectations (Amipara et al., 2020; Sheela & Venkatesh, 2015). Additionally, trouble with lactation was found to increased feelings of dissatisfaction, guilt, and low self-efficacy amongst mothers (Amipara et al., 2020; Sheela & Venkatesh, 2015). The study conducted by Amipara et al. (2020) found that the median duration of breastfeeding ranged from 26-29 weeks in depressed mothers compared to the average of 39 weeks in non-depressed mothers. This may have been because of low interest and motivation in depressed mothers leading to decreased intention to feed their baby, resulting in infant malnutrition (Amipara et al., 2020). Parity, primigravida, and unplanned or unwanted pregnancy, were found to be significant risk factors (Agarwala et al., 2019; Mishra et al., 2020; Suguna et al., 2015). The study conducted by Agarwala et al. (2019) found that having more than two children and a history of pregnancy loss increased the risk of PPD by three and four times, respectively. This may be due to stressors associated with pregnancy loss or insufficient coping resources leading to increased anxiety and fear during future pregnancies (Giannandrea et al., 2013). Furthermore, unplanned or unwanted pregnancy was found to be associated with increased risk for PPD in some studies in the sample, which may be justified by differences in the region (Patel et al., 2015; Sherkhane & Sharma., 2019). Mothers in urban slums may have additional difficulty supporting an unplanned child due to poverty, whereas mothers in rural areas may have higher SES and familial support (Sherkhane & Sharma., 2019; Suguna et al., 2015). Psychological FactorsEight studies discussed psychological factors such as personal experiences of pregnancy, labor, and family history of psychological disorders. Prior history of familial psychiatric disorders was found to be associated with risk factors of PPD due to genetic inheritance of mental illnesses (Suguna et al., 2015). However, not all of the studies agreed that family history was a significant risk factor (Javalkar &Vanitha, 2018; Mishra et al., 2020). This disagreement may be justified by the lack of mental health awareness and adequate measurement tools in previous generations, resulting in underreported mental health problems in families. Mothers who described their experience post-labor as “stressful” were more likely to display depressive symptoms (Kale et al., 2019). Furthermore, women who had severe mood swings and low self-esteem during the antenatal period were likely to be at risk for PPD (Javalkar &Vanitha, 2018; Johnson et al., 2015). This may be due to antenatal depression or other underlying psychiatric illnesses that went undiagnosed and continued postpartum. Undiagnosed mental illness may be explained due to the difference in the quality of life, awareness, and stigma about mental health in differing regions. It is integral to look at psychological risks because suicidal ideation was reported to be an outcome in mothers with depressive symptoms (Javalkar &Vanitha, 2018; Sheela & Venkatesh, 2015). Cultural and Spousal FactorsOnly two out of the eight studies that analyzed cultural factors as a risk to PPD found gender of the child as significant. Disappointment with a female child after familial and personal expectations of a son may explain this association with PPD. Additionally, sons may be preferred for religious reasons, as eighty percent of India’s population is Hindu (Census of India: Religion, 2001). In Hinduism, women cannot complete the ideal Hindu life cycle by obtaining “moksha” or redemption as they are prevented from performing the obligatory prayers during their menstrual cycle (Rao et al., 2015). The expectations for a son may lead to a build-up of social pressure, contributing to the depressive symptoms if a daughter is born. Furthermore, societal pressures and expectations of having a son may lead to female infanticide and feticide, which has become prevalent in regions of South India, such as Tamil Nadu, where the birth of a daughter was found to be associated with increased risk of PPD (Rao et al., 2015; Sheela & Venkatesh, 2015). The studies analyzed disagreed on whether religion or culture is associated with PPD, which may be due to religious differences amongst regions as it was not defined if populations were Hindu, Muslim, or Christian. Two studies found that domestic abuse and marital problems were risk factors for PPD (Patel et al., 2015; Sheela & Venkatesh, 2015). However, Suguna et al. (2015) concluded that marital disharmony was not a risk factor. This disagreement may be justified due to underreported domestic abuse as women may be fearful of financial deprivation as a result of leaving their abusive husbands (Rao et al., 2015). This anxiety may create fear for themselves and their children’s livelihood, thereby explaining the association with PPD. Furthermore, women are found to be defensive when questioned about marital problems or abuse. This may occur due to the common cultural practice of pathibhakti (which can be translated from Hindi as utmost loyalty and devotion to one’s husband) (Chandran et al., 2002). Additionally, it was found that parity increased the risk of PPD (Agarwala et al., 2019; Patel et al., 2015). This may be explained by the lack of control women have over their own fertility due to a patriarchal society (Patel et al., 2015). Thus, women will typically continue to conceive until a son is born, which can be considered a form of sexual abuse. Socio-demographic FactorsAll ten studies discussed the impact of socio-demographic factors such as age, education, marital status, type of housing, and relationship with extended family as potential risk factors of PPD. Advanced maternal age was a significant factor in only two studies (Patel et al., 2015; Sherkhane & Sharma., 2019). Higher maternal age increases the risk of obstetric complications, justifying the association between age and risk of PPD (Aasheim et al., 2012). The disagreement amongst studies concerning advanced maternal age as a risk factor may be due to the low representation of different age groups in samples. Although maternal education was found to be a potential risk factor for PPD in three studies, it was not clear if higher or lower levels of education were correlated to risk (Agarwala et al., 2019; Amipara et al., 2020; Mishra et al., 2020). Mishra et al. (2020) found that education below the primary school level was significantly associated with PPD. Thus, a lack of sexual, financial, and general education may increase the risk of PPD. Conversely, Agarwala et al. (2019) determined that higher levels of education were associated with a greater prevalence of PPD as women may be aware of mental illness and can seek help when required. The other studies did not find education to be a risk factor. This inconsistency may be because studies that agreed with age as a factor recruited subjects from community centers, whereas the other studies used hospital centers. Community centers may have a more diverse population due to lower financial costs, whereas hospitals may be more likely to obtain patients who can afford medical care. Furthermore, there is a discrepancy between all studies on whether SES was correlated with a higher risk of PPD. This difference may have occurred because of small sample sizes obtained from the immediate region around a single hospital rather than multiple medical centers where SES may have been more diverse. Moreover, the living arrangements and the relationship with in-laws were also found to be associated with higher risks for PPD in some studies (Javalkar &Vanitha, 2018; Mishra et al., 2020; Suguna et al., 2015). Mishra et al. (2020) determined that the risk of PPD was higher in mothers who lived in a joint family and had a poor relationship with their in-laws. It was found that living in a nuclear family reduced the risk of depressive symptoms by a factor of eleven because of lower familial expectations and tension (Patel et al., 2015). Conversely, residing in a nuclear family, was found to increase the risk of PPD as it increased the responsibility and isolation felt by the mother (Javalkar &Vanitha, 2018). It has been found that life satisfaction during the post-natal period is higher when the mother is surrounded by family and friends who can support her (Munaf & Siddiqui, 2013). However, a lower risk of PPD resulting from a joint family arrangement may be hindered by a poor relationship with in-laws as it increases stress within the home. This would justify why the studies in the sample disagreed whether the type of living arrangement is a significant risk factor. Additionally, studies that did not have this association also had differences in regional settings, as joint families may be more prevalent in rural areas than urban regions (Singh, 2003). DiscussionThis critical analysis aims to provide a comprehensive and updated understanding of PPD in India using recently published studies. Ten studies from various regions were analyzed and summarized. There was an extensive prevalence range of PPD (7% - 48%) amongst the studies. The studies investigated similar variables, categorized as biological/obstetric, psychological, cultural, and socio-demographic risk factors. Most existing literature based in Western populations agrees that perinatal depression may be a result of factors such as childcare stress, psychiatric illness, obstetric complications, stressful life events, marital dissatisfaction, lack of social and familial supports, unwanted pregnancies, and low SES (Lanes et al., 2011; O’hara & Swain, 1996; Pearlstein et al., 2009). However, there was disagreement amongst the analyzed studies on which factors significantly increased the risk of PPD. This may have resulted due to geographic differences such as variance between rural and urban populations and the quality of maternal care provided. In addition, there are limited sources exploring the cultural and religious impacts on PPD since researchers have tended to focus on the psychosocial and biological variables as they are more easily measured, more concrete, and viewed as valid in comparison to more abstract factors like culture. It is essential to understand the interplay between cultural practices with biopsychosocial variables in order to reduce rates of PPD in India. Understanding all the variables impacting PPD is essential as it will influence the formulation of policies and interventions that are tailored to specific cultures, which may make mothers feel more comfortable seeking help as the societal stigma and shame associated with mental health will be acknowledged and considered. LimitationsThere are several limitations in the studies analyzed in this paper. Majority of the papers have a small sample size reducing the result’s generalizability. Papers selected a population that was centered around a single medical or community center rather than multiple locations. Therefore, data only represented a single population rather than a diverse one; thereby, decreasing the sample’s representativeness. In addition, the studies collected data over different postnatal periods, which may impact the results found. Furthermore, the self-reported measurement tools were translated from English without discussing the validity of the translations. Likewise, the cutoffs for the EPDS in the studies varied, which may impact the results. Additionally, underreported domestic violence and attenuated feelings regarding PPD due to the presence of spouses or family members during the time of checkups and the fear of the stigma associated with depression may increase bias. Additionally, the paper by Sherkhane & Sharma. (2019) should be mentioned as a specific limitation for this study since it did not use the EPDS, which may impact the overall results as populations were not assessed using the same standardized tool. Moreover, the studies examined were only included if they were in English. This may have left out other studies that could have provided valuable insight. Lastly, the studies selected did not undergo quality assessment, which may influence this paper’s the internal validity. ConclusionThis paper aimed to understand the various risk factors associated with PPD. The extensive range in prevalence rates indicates sparsity in PPD awareness, management, and treatment. The papers analyzed conflicted with each other on variables associated with PPD, preventing a definitive list of risk factors from being established. This may have been due to limitations in individual study designs, small populations, and regional cultural differences. To gain a clearer understanding of PPD in India, research should focus on cultural variables along with biopsychosocial factors. Research should be conducted on a national level, using large population samples from across the country rather than samples from single medical and community centers. This type of study design would better illustrate the current national prevalence. It may also help to gain a direct understanding of the regional and cultural differences in PPD rates by comparing the southern, northern, eastern, and western states as well as rural and urban populations in each region. Lastly, in addition to quantitative data like the national prevalence, qualitative data about women’s lived experiences with PPD is needed to formulate culturally sensitive intervention plans. Furthermore, it is vital that health care professionals can recognize early symptoms and provide management techniques in a timely manner. Due to India’s focus on joint families, interventions involving the entire family may be more beneficial (Linsu et al., 2018). This may also give health care professionals a chance to correct misconceptions and stereotypes about mental health; thereby, reducing the stigma that family members hold. It is also integral to provide three levels of prevention: primary, secondary, and tertiary, thereby preventing the onset of PPD by reducing its risks and attenuating complications of existing PPD patients. The primary method should aim to reduce stigma, provide education about mental health, and provide family planning resources on a community level (Sherkhane & Sharma., 2019). The secondary intervention should include early detection of PPD by assessing antenatal symptoms and doing routine screening using self-reported tools such as the EPDS during antenatal checkups (Johnson et al., 2015; Mishra et al., 2020; Patel at al., 2015). Lastly, tertiary interventions should prevent relapse of symptoms through regular check-ins with mothers during the postnatal period (Klainin & Arthur, 2009). This paper provides an understanding of the current literature and the lack of agreement regarding potential risk factors of PPD in India. It will be essential to gather data on perinatal depression and its risk factors across India to provide mothers the help they need by informing policymakers and medical professionals of suitable interventions. Further evidence may encourage the government to fund the research required to reduce the encumbrance of postpartum depression, thereby ensuring that mothers can seek help without the shame or stigma associated with mental illness. ReferencesAasheim, V., Waldenström, U., Hjelmstedt, A., Rasmussen, S., Pettersson, H., & Schytt, E. (2012). Associations between advanced maternal age and psychological distress in primiparous women, from early pregnancy to 18 months postpartum. BJOG: An International Journal of Obstetrics & Gynaecology, 119(9), 1108–1116. https://doi.org/10.1111/j.1471-0528.2012.03411.x Agarwala, A., Arathi Rao, P., & Narayanan, P. (2019). Prevalence and predictors of postpartum depression among mothers in the rural areas of Udupi Taluk, Karnataka, India: A cross-sectional study. Clinical Epidemiology and Global Health, 7(3), 342–345. https://doi.org/10.1016/j.cegh.2018.08.009 Amipara, T., Baria, H., & Nayak, S. (2020). A study on postpartum depression and its association with infant feeding practices and infant nutritional status among mothers attending the anganwadi centers of Valsad district, Gujarat, India. Indian Journal of Community Medicine, 45(3), 299. https://doi.org/10.4103/ijcm.ijcm_171_19 Census of India: Religion. (2001). Censusindia.Gov.In. https://censusindia.gov.in/census_And_you/religion.aspx Chandran, M., Tharyan, P., Muliyil, J., & Abraham, S. (2002). Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. British Journal of Psychiatry, 181(6), 499–504. https://doi.org/10.1192/bjp.181.6.499 Chandra P. S. (2004). Post-partum psychiatric care in India: the need for integration and innovation. World psychiatry : official journal of the World Psychiatric Association (WPA), 3(2), 99–100. Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of Postnatal Depression.British Journal of Psychiatry, 150(6), 782–786. https://doi.org/10.1192/bjp.150.6.782 Field, T. (2010). Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior and Development, 33(1), 1-6. doi:10.1016/j.infbeh.2009.10.005 Fisher, J., Cabral de Mello, M., Patel, V., Rahman, A., Tran, T., Holton, S., & Holmes, W. (2011). Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization, 90(2), 139-149H. https://doi.org/10.2471/blt.11.091850 Ghaedrahmati, M., Kazemi, A., Kheirabadi, G., Ebrahimi, A., & Bahrami, M. (2017). Postpartum depression risk factors: A narrative review. Journal of Education and Health Promotion, 6. https://doi.org/10.4103/jehp.jehp_9_16 Giannandrea, S. A. M., Cerulli, C., Anson, E., & Chaudron, L. H. (2013). Increased Risk for Postpartum Psychiatric Disorders Among Women with Past Pregnancy Loss. Journal of Women’s Health, 22(9), 760–768. https://doi.org/10.1089/jwh.2012.4011 Gupta, S., Kishore, J., Mala, Y. M., Ramji, S., & Aggarwal, R. (2013). Postpartum Depression in North Indian Women: Prevalence and Risk Factors. The Journal of Obstetrics and Gynecology of India, 63(4), 223-229. doi:10.1007/s13224-013-0399-x Javalkar, S., & Vanitha, S. (2018). A Study on Postnatal Depression among Women Attending Tertiary Care Hospital in Davanagere, Karnataka. National Journal of Community Medicine, 9(3), 167–171. https://www.bibliomed.org/?mno=282791 Johnson, A., Edwin, S., Joachim, N., Mathew, G., Ajay, S., & Joseph, B. (2015). Postnatal Depression among women availing maternal health services in a rural hospital in South India. Pakistan Journal of Medical Sciences, 31(2). https://doi.org/10.12669/pjms.312.6702 Kale, D. P., Tambawala, Z. Y., & Rajput, N. M. (2019). Journal of South Asian Federation of Obstetrics and Gynaecology. Journal of South Asian Federation of Obstetrics and Gynaecology, 11(4), 239–242. https://doi.org/10.5005/jp-journals-10006-1696 Klainin, P., & Arthur, D. G. (2009). Postpartum depression in Asian cultures: A literature review. International Journal of Nursing Studies, 46(10), 1355–1373. https://doi.org/10.1016/j.ijnurstu.2009.02.012 Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x Kumar, P., & Dhillon, P. (2020). Length of stay after childbirth in India: a comparative study of public and private health institutions. BMC Pregnancy and Childbirth, 20(1). https://doi.org/10.1186/s12884-020-2839-9 Lanes, A., Kuk, J. L., & Tamim, H. (2011). Prevalence and characteristics of Postpartum Depression symptomatology among Canadian women: a cross-sectional study. BMC Public Health, 11(1). https://doi.org/10.1186/1471-2458-11-302 Linsu, T., Sailaxmi, G., & Jithin Thomas, P. (2018). Interventions for Mothers with Postpartum Depression: A Systematic Review. International Journal of Depression and Anxiety, 1(1). https://doi.org/10.23937/ijda-2017/1710002 Mishra, K., Mohapatra, I., & Rout, R. N. (2020b). An epidemiological study on depression among women during postpartum period in an urban slum of Bhubaneswar.Journal of Family Medicine and Primary Care,9(9), 4736–4740. https://doi.org/10.4103/jfmpc.jfmpc_793_20 Munaf, S., & Siddiqui, B. (2013). Relationship of Post-natal Depression with Life and Marital Satisfaction and Its Comparison in Joint and Nuclear Family System. Procedia - Social and Behavioral Sciences, 84(9), 733–738. https://doi.org/10.1016/j.sbspro.2013.06.636 O’hara, M. W., & Swain, A. M. (1996). Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry, 8(1), 37–54. https://doi.org/10.3109/09540269609037816 Patel, H. L., Ganjiwale, J. D., Nimbalkar, A. S., Vani, S. N., Vasa, R., & Nimbalkar, S. M. (2015). Characteristics of Postpartum Depression in Anand District, Gujarat, India. Journal of Tropical Pediatrics, 61(5), 364–369. https://doi.org/10.1093/tropej/fmv046 Pearlstein, T., Howard, M., Salisbury, A., & Zlotnick, C. (2009). Postpartum depression. American Journal of Obstetrics and Gynecology, 200(4), 357–364. https://doi.org/10.1016/j.ajog.2008.11.033 Rahman, A., Iqbal, Z., & Harrington, R. (2003). Life events, social support and depression in childbirth: Perspectives from a rural community in the developing world. Psychological Medicine, 33(7), 1161-1167. https://doi.org/10.1017/s0033291703008286 Rao, G. P., Vidya, K. L., & Sriramya, V. (2015). The Indian "girl" psychology: A perspective. Indian journal of psychiatry, 57(Suppl 2), S212–S215. https://doi.org/10.4103/0019-5545.161480 Sheela, C. N., & Venkatesh, S. (2015). Screening for Postnatal Depression in a Tertiary Care Hospital.The Journal of Obstetrics and Gynecology of India,66(S1), 72–76. https://doi.org/10.1007/s13224-015-0766-x Sherkhane, M. S., & Sharma., P. (2019). Depression in postpartum women residing in urban slums using Patient Health Questionnaire-9. International Journal of Medical Science and Public Health, 8(4), 286–291. https://doi.org/10.5455ijmsph.2019.11337201802032019 Singh, J. P. (2003). Nuclearisation of Household and Family in Urban India.Sociological Bulletin, 52(1), 53–72. https://doi.org/10.1177/0038022920030103 Suguna, A., Naveen, R., & Surekha, A. (2015). Postnatal Depression Among Women Attending a Rural Maternity Hospital in South India. National Journal of Community Medicine, 6(3). https://doi.org/pISSN 0976 3325 Thippeswamy, H., Desai, G., & Chandra, P. (2018). Help-seeking patterns in women with postpartum severe mental illness: a report from southern India.Archives of Women’s Mental Health,21(5), 573–578. https://doi.org/10.1007/s00737-018-0830-5 Upadhyay, R. P., Chowdhury, R., Aslyeh Salehi, Sarkar, K., Singh, S. K., Sinha, B., Pawar, A., Rajalakshmi, A. K., & Kumar, A. (2017). Postpartum depression in India: a systematic review and meta-analysis.Bulletin of the World Health Organization,95(10), 706-717C. https://doi.org/10.2471/blt.17.192237 Williams, A., Sarker, M., & Ferdous, S. T. (2017). Cultural Attitudes toward Postpartum Depression in Dhaka, Bangladesh.Medical Anthropology,37(3), 194–205. https://doi.org/10.1080/01459740.2017.1318875 Wisner, K. L., Moses-Kolko, E. L., & Sit, D. K. Y. (2010). Postpartum depression: a disorder in search of a definition.Archives of Women’s Mental Health,13(1), 37–40. https://doi.org/10.1007/s00737-009-0119-9 Wisner, K. L., Sit, D. K. Y., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., Eng, H. F., Luther, J. F., Wisniewski, S. R., Costantino, M. L., Confer, A. L., Moses-Kolko, E. L., Famy, C.S., & Hanusa, B. H. (2013). Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum Women With Screen-Positive Depression Findings.JAMA Psychiatry,70(5), 490. https://doi.org/10.1001/jamapsychiatry.2013.87 Suggested Reading from Inquiries Journal
Inquiries Journal provides undergraduate and graduate students around the world a platform for the wide dissemination of academic work over a range of core disciplines. Representing the work of students from hundreds of institutions around the globe, Inquiries Journal's large database of academic articles is completely free. Learn more | Blog | Submit Latest in Sociology |